The moment a doctor breaks bad news, like a spine surgery, everything changes. After years of getting medications and physical therapy for chronic back pain, surgery seems like a last hope. But you also start questioning whether it’s good or not, including concerns about the spine surgery success rate in elderly patients. Is it necessary? Will it work?
That’s where the spine surgery statistics in the United States are important to understand. Although many people who undergo spine surgery experience improvement in their symptoms, the success rate varies widely depending on a variety of factors.
The purpose of this article is to cut through the noise by providing you with some straightforward, unbiased statistics about spine surgery in the United States, so you will understand what “success” actually means, how often outcomes fall short, and what risks are usually ignored.
Back Surgery Statistics and the Risk Assessment
According to the Journal of Surgical Case Reports, initial spinal surgeries have a success rate of about 50%. However, the success rate for patients who have a second, third, or fourth back surgery diminishes dramatically. Only 30%, 15%, and 5% of patients had successful outcomes from these operations.
The truth of the matter is that back surgery is a risky procedure. Some of the complications that can be expected include infections, nerve damage, failed back surgery syndrome, and blood clots. Although the back surgery death rate is indeed low, it is not nonexistent, especially among seniors. Nonfatal complications can also last for a lifetime.
So, why is the actual spine surgery success rate often below what patients would expect? Success is usually defined by a reduction in pain in the near term, rather than by long-term function. This means that many patients are not prepared for an outcome that does not meet their expectations, particularly those dealing with chronic neck pain or long-standing nerve-related symptoms.
Analyzing the Spinal Fusion Success Rate
Spinal fusion is a surgical procedure that unites two or more spinal vertebrae. The primary goal of the procedure is to eliminate the unpleasant mobility between vertebrae, thereby providing stability and alleviating discomfort.
According to the Neurosurgeons of New Jersey, the spinal fusion success rate is generally between 70% and 90%. This figure varies depending on the underlying ailment and the doctor’s surgical method. Outcomes vary by anatomy, while the L4-L5 spinal fusion success rate is likely higher than that of multi-level fusions.
Another critical factor often downplayed is age. Generally, the spinal fusion success rate in the elderly is observed to be lower owing to reduced bone density and decreased healing rates, which increases the chances of complications and reduces the likelihood of lasting lower back pain relief.
What Determines the Spinal Surgery Success Rate?
Spine surgery success rate depends on the following factors.
- The type of spinal surgery: Success percentages vary. Minimally invasive operations, for example, are more likely to succeed and recover faster than standard open surgeries.
- The patient’s overall condition: A patient’s health, including any pre-existing medical issues, can affect the success of surgery. Healthier people often get better results.
- The severity of the spinal condition: The more serious the spinal problem, the more difficult the surgery may be. Patients with less severe illnesses typically have higher success rates. Some people suffer from chronic sciatica pain caused by spinal problems that, in some situations, necessitate surgical intervention when conservative therapy fails.
- Surgeon Expertise: The surgeon’s competence and experience are critical to the outcome of the operation. Experienced spine surgeons are more likely to produce positive outcomes.
- Age considerations: There is often an age limit for spinal surgery, which can affect the choice and outcome of surgical intervention.
The Reality of Failed Back Surgery Syndrome (FBSS)
Failed Back Surgery Syndrome (FBSS) is a complex illness characterized by chronic or recurring pain after spine surgery. Patients with FBSS frequently endure low back pain, leg pain, or both, even after undergoing operations such as spinal disc herniation repair or other neurosurgical therapies. This syndrome can have a major influence on a person’s quality of life, necessitating a multidisciplinary approach for effective treatment.
Recognizing the indications and symptoms of failed back surgery syndrome (FBSS) is critical for early intervention and effective care. Patients may also report radiating leg discomfort, which might be due to issues with the intervertebral disc or spinal cord.
It affects 20-40% of people undergoing spinal surgery, making it a major issue in the area of orthopedics. The occurrence of FBSS varies according to the type of surgery performed, the patient’s characteristics, and the diagnostic criteria used.
Proven Non-Surgical Alternatives to Back Surgery
There are different safe alternatives to back surgery. Some of them are:
Spinal Decompression
Spinal decompression therapy does not usually require pain medication. The procedure is not only safe and painless, but also comfortable and soothing.
The non-surgical spinal decompression therapy consists of around 20 treatment sessions spread over 4-6 weeks. Each operation uses a unique physiotherapeutic device and is performed by a certified physician specializing in spinal decompression for disc issues. The treatment sessions are quick, lasting around 30-45 minutes.
CBP Therapy
The CBP Technique, also known as Chiropractic BioPhysics (CBP), emphasizes ideal posture and spinal alignment as the primary aims of chiropractic care, while also documenting improvements in pain and functional outcomes. By restoring the standard spinal structure, CBP represents a form of structural chiropractic care that can provide a more lasting solution than surgery for some mechanical and postural issues.
Functional Medicine
The functional medicine approach addresses the fundamental cause of symptoms. It targets hidden culprits such as chronic inflammation, nutritional deficiencies, and metabolic imbalances, which often cause long-term discomfort and make surgery seem unavoidable when it isn’t.
For many patients, functional medicine for chronic pain helps reduce long-term discomfort and makes surgery seem unavoidable when it isn’t.
At Thrive, our philosophy is very simple: We like to fix what is wrong, rather than just cutting out what hurts. While surgeries often remedy what is visible on imaging studies, pain is never caused by a single factor. This is why so many of our patients experience relief through non-surgical means that work.
Make an Informed Choice for Your Spine
When you look past the headlines and at the actual spine surgery success rate, one truth is evident: surgery is not always the best or even the first option. While spinal surgery is beneficial for certain patients, the statistics for spinal surgery point to mixed results, substantial risk of complications, and too many patients left with pain after surgery.
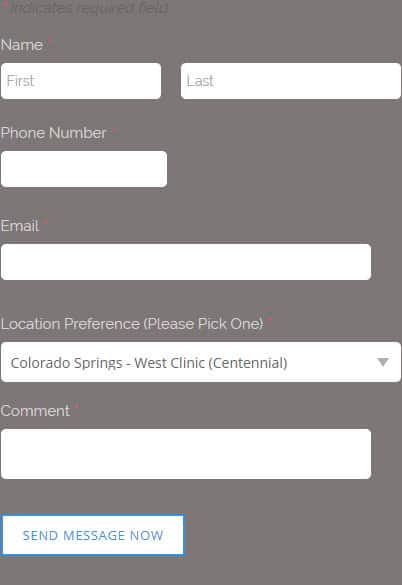
Before opting for a surgical procedure, you must understand what is causing you pain. At Thrive Health Systems, we use the latest technology in conjunction with other modalities to make a treatment Plan.
If you or someone you know is thinking about spinal surgery or believes it’s their only hope, don’t hesitate to consult with Thrive Health Systems.